Patient's Guide to Anesthesia~For patients undergoing anesthesia and their families~
About the Patient's Guide to Anesthesia
The Patient's Guide to Anesthesia contains easy to understand information about anesthesia for patients and their families. If you have any questions, please discuss them with your anesthesiologist. Here we provide step-by-step explanations of anesthesia for you and your family.
Table of contents
1. What is anesthesia?
2. Who is an anesthesiologist?
3. Types of anesthesia
4. What happens before, during and after anesthesia?
5. Complications of anesthesia
6. Emergency medical procedures
Afterword
For the guardians of children undergoing anesthesia
Children also require anesthesia when they undergo surgery or medical procedure. Their bodies, organ function, psychological characteristics, and other traits differ from those of adults and, thus, require special consideration.
Special considerations for children will be additionally described in each section of this handbook.
1. What is anesthesia?
Most surgeries necessitate a cut made through the skin, and therefore are, painful and stressful without anesthesia. Pain and stress can impact the recovery after surgery or medical procedure.
Anesthesia reduces the pain and stress of surgery and procedures which can potentially impact safety and recovery from surgery. The goal of anesthesia is to keep the patient safe and comfortable during surgery or a medical procedure.
2. Who is an anesthesiologist?

Your anesthesiologist is responsible for your comfort, safety and overall condition before, during and after the surgical or medical procedure. To achieve this, the anesthesiologist manages the vital functions of your body including circulation, respiration and pain.
Circulation - blood pressure, pulse rate, urination, and other heart and blood-related issues.
Respiration – oxygen, respiratory rate, mechanical ventilation, and body fluid balance.
Pain – Your anesthesiologist relieves your pain using anesthetics. Pain affects your recovery after surgery.
If you are experiencing any pain after the surgery, don’t just struggle through it. Seek attention from your medical team.
3. Types of anesthesia
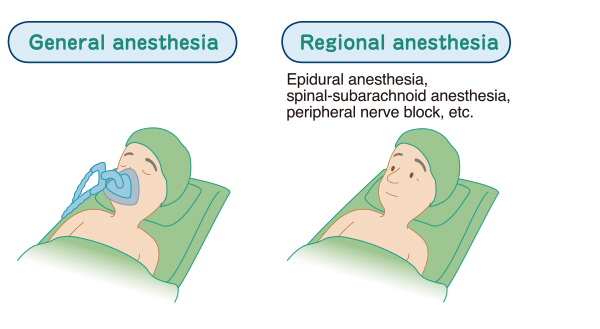
General anesthesia
(see Performing anesthesia and operation-General anesthesia for details)
Regional anesthesia
Epidural anesthesia, spinal anesthesia, peripheral nerve block, etc.
(see Performing anesthesia and operation-Regional anesthesia for details)
General or regional anesthesia can be used alone or in combination. With regional anesthesia, you are sometimes put into light sleep (sedation). During surgery, the method of anesthesia might be changed depending on your overall conditions.
Your anesthesiologist will choose the most appropriate method for you.
General anesthesia is used for surgeries for the abdomen, chest, spine, jaw, and/or face. Regional anesthesia is mainly used for minor surgeries, and surgeries for arms and legs.
For surgeries performed below the navel, such as surgeries for obstetrics/gynecology, appendicitis, hemorrhoids, or lower limb fractures, spinal or epidural anesthesia is typically chosen alone. However, these forms of regional anesthesia can be combined with general anesthesia depending on the procedure and the patient’s condition.
For children…
Surgeries and some procedures on a child or a baby are usually performed under general anesthesia. Anesthesia eliminates any anxiety or fear during the operation and enables doctors to perform the procedure while they are asleep. However, regional anesthesia may carefully be selected for short surgeries or procedures on a child who is able to understand what is happening to him or her.
4. What happens before, during and after anesthesia?
1. Your medical team, including your anesthesiologist, will help you prepare for anesthesia.
● Interview and examination by an anesthesiologist before surgery (pre-anesthesia clinics)
Your anesthesiologist does a preoperative interview and examination to assess your condition before surgery and to select appropriate anesthesia and analgesia.
For children…
Please let your anesthesiologist know about the condition of your child's health, particularly about any past or present health issues, such as cough, running nose, asthma, allergies, heart disease, or epilepsy, and any medications or other considerations you are aware of.
-
Have you or a family member ever undergone anesthesia or surgery?
If so, did you or your family member experience malignant hyperthermia or anything else abnormal? - Do you have any diseases involving major organs, such as the heart, kidneys, lungs, or brain?
- Are you regularly taking any medication? For example, blood pressure medication, diabetes medication, drugs to prevent blood clotting, steroids, etc.
- Do you have a history of asthma?
- Do you tend to get nosebleeds or experience bleeding that is difficult to stop?
- Are you susceptible to allergies or do you need any medical considerations which you were told to let a new doctor know about?
- Have you get vaccinated recently?
- Do you have any loose or weak teeth? Do you use dentures?
- Do you have shoulder or arm pain that occurs when you bend your neck?
- Can you open your mouth widely?
- Do you have any trouble talking or hearing?
- Have you had eye surgery (glaucoma, cataracts) recently?
- Are you pregnant, or do you have any chance of being pregnant?
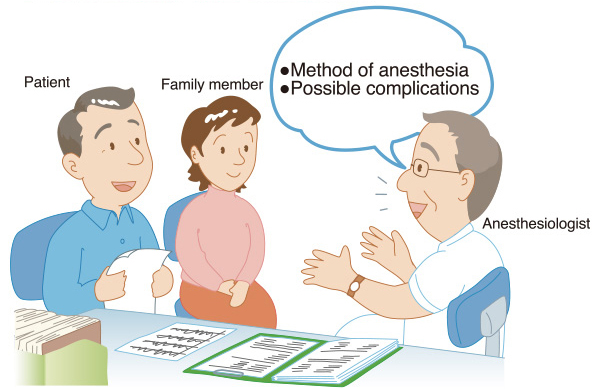
● Informed consent for anesthesia
After obtaining information about the patient’s general condition, medical history, and upcoming surgery, your anesthesiologist will propose a suitable anesthesia method and explain it to you, and if necessary, to your family, next to kin or your delegate.
● Instructions before anesthesia
It is extremely important that you follow these instructions from your anesthesiologist to ensure your safety during anesthesia.
Refraining from eating and drinking
While under anesthesia, any food or liquid remaining in the stomach could be vomited up. This food or liquid could enter your airway and you could develop a life-threatening choking and severe pneumonia. You must NOT eat or drink anything for a certain period before your surgery or procedure.
Smoking
We strongly encourage patients to stop smoking once your surgery is anticipated. Smokers experience more coughing and phlegm after surgery, which can lead to pneumonia or worse wound pain.
Also, smokers have a higher rate of infection after surgeries, and their wounds take a longer time to heal.
Your surgery may be postponed if you have a fever from the common cold or other causes.
For children…
You and your family members must not give any food or drink to your child unless your anesthesiologist specifically approves it even if your child becomes upset or complain about being hungry or thirsty. All preoperative instructions from your anesthesiologist need to be followed for your child’s safety. Please refrain from smoking in front of your child(ren) at all times.
● Moving to the operating room
Before going to the operating room, you may be given medications or injections for pre-anesthetic purpose. As these medications can make you dizzy, please follow instructions from your medical team.
For children…
Before the surgery, your child may be given medication or a suppository to relieve his or her anxiety.
To make him or her feel more at ease, a guardian sometimes may be asked to accompany the child.
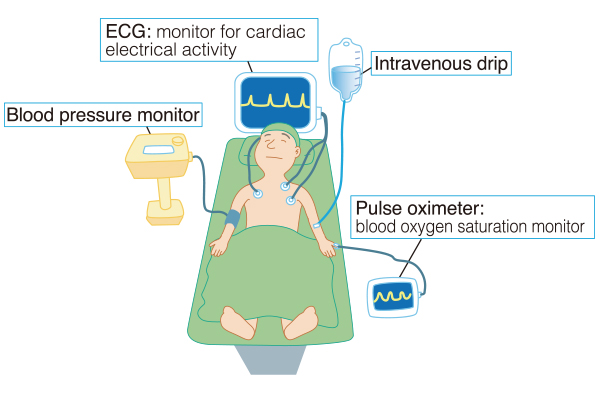
After entering the operating room, the team will confirm your identity (e.g. your name, date of birth, and hospital ID). Next, all the monitoring devices (ECG, blood pressure device, etc.) will be applied to you as well as the intravenous line(s) before anesthesia. These devices will remain attached during and after the surgery.
General anesthesia
1. Starting anesthesia
You are given oxygen through a face mask that covers your nose and mouth. Relax, and take deep breaths. The sleep medications are given in IV fluid and/or oxygen, and will get you asleep quickly.
2. Inserting the breathing tube
A tube for breathing, endotracheal tube or a laryngeal mask, is inserted via your mouth to give you enough oxygen safely. This procedure can damage loose or weakend teeth. If you are concerned about any of your teeth, please tell your medical team before the anesthesia.
3. Surgery
During the surgery, your anesthesiologist monitors you taking in to account the progress of the surgery to maintain your optimal condition during the procedure. To achieve this, your anesthesiologist assesses your condition every moment and adjusts the medications, mechanical ventilation, and IV fluid or blood transfusions as needed.
- If regional anesthesia is not being used, continue to 4. After surgery.
For children…
If an IV line is already present, your child will be given anesthetic medication by IV. When there is no IV line, anesthetic gas via a face mask will be used. Breathing this gas for 1–2 minutes will make your child sleep deeply so that an IV line can be placed without any pain or stress. As a normal response to anesthetics, some children become overexcited for a short duration of time before going off to sleep.
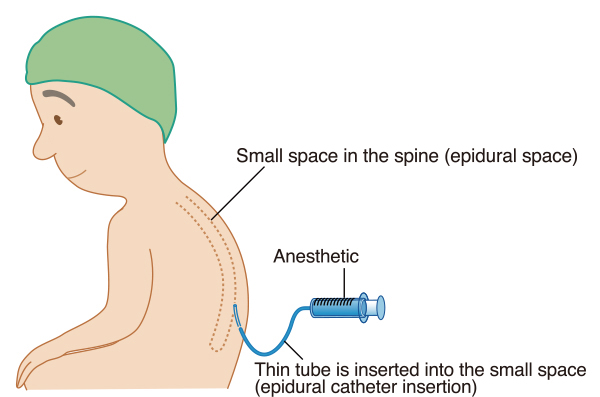
Local anesthetics are given into the epidural space, which is located close to the spinal cord in your back. This method is used to reduce pain in the area being operated.
Based on the surgical area, your anesthesiologist determines the location where the local anesthetic is injected into the epidural space. The anesthetic is injected via a thin tube, called a catheter.
For the catheter insertion, you will arch your back forward like an angry cat. After disinfecting the area, a local numbing medicine will be injected in your back skin, which will make the procedure almost entirely painless.
Epidural anesthetics may be administered after the surgery if a catheter left in place for post-operative pain relief. Post-operative epidural anesthetics can be very effective at relieving pain. The catheter will be taken out several days after the surgery.
In spinal anesthesia, your anesthesiologist will insert a thin needle in to your back to add local anesthetic to cerebrospinal fluid, directly anesthetizing the spinal cord. During the time the anesthesia is working (3–6 hours), you will lose sensation, and your legs will be numb and unable to move. The body positioning, disinfection methods, and initial local numbing injection for spinal anesthesia are the same as those for epidural anesthesia.
Some patients experience headaches after spinal anesthesia; however, this is rare. Normally, this disappears after a few days of rest.
If your headache persists or worsens, please contact your medical team as soon as possible to rule out other causes and for further treatment.
Peripheral nerve block
This method eliminates pain in an area by injecting a local anesthetic along the pathway of a nerve. This method anesthetizes a smaller area than epidural or spinal anesthesia, with the purpose of only anesthetize the smallest area necessary.
For some surgeries, a peripheral nerve block can be used alone. A peripheral nerve block also can be combined with general anesthesia and normal painkillers after surgery.
Nerve blocks of the upper limbs are performed by inserting a needle on the side of the neck, in the armpit, or near the collarbone. For the lower limbs, a needle is inserted in the groin, buttocks or legs. The local anesthetic is injected while the needle tip is monitored with ultrasound, electrical stimulation, or X-ray.
4. After surgery
With general anesthesia, at the end of surgery, your anesthesiologist stops giving anesthetics. How long it takes you to wake up depends on the surgery, anesthesia, and your condition. When you begin to wake up, your anesthesiologist will speak to you. You will hear directions such as – open your eyes, or squeezing your hand.
Note that you may have difficulty in speaking for a while, even after the tube is removed from your mouth.
Your anesthesiologist will continue to monitor you, especially your blood pressure, pulse rate, respiration, and blood oxygen levels.
Before returning to your room, you may spend some time in the post-anesthesia care unit (PACU), or the intensive care unit (ICU), depending on your condition.
5. Return to the hospital ward
● After general anesthesia, it will take some time to wake up fully. Your family should not be worried if you continue to sleep or move unusually.
Without general anesthesia or sedation, you will be most likely able to talk with somebody immediately when you return to your room. If general anesthetics or sedatives were used , it might take additional time to wake up completely.
● With regional anesthesia, the areas effected may continue to feel numb, even after returning to your room. This will generally disappear in a few hours.
● Depending on the type of surgery or anesthesia, you may feel pain immediately after waking up from anesthesia. Intravenous or oral painkillers are available for you, according to your condition. Please call your medical team , and seek help to alleviate your pain.
● Patient-controlled analgesia (PCA) is a pain relief option. It is a device that patients can activate by themselves to help control pain. When your pain is severe, you can push a button to safely administer painkillers through an epidural catheter or intravenous line. The device is designed not to give an excessive dose. If you feel any discomfort when using a PCA or if your family sees your breathing pattern being dangerously suppressed, please notify your medical team immediately.
● You may experience a buildup of phlegm after the surgery, particularly with general anesthesia. This can cause lung problems, such as pneumonia or atelectasis. Taking deep breaths, coughing and using incentive spirometry can prevent these problems. If pain makes it hard for you to cough or breathe deeply, please tell your medical team so that they relieve your pain in a timely manner.
5. Complications of anesthesia
Loose or missing teeth
Placement of an endotracheal tube or a laryngeal mask, as well as grinding of the teeth when waking up, may damage your teeth or dentures.
Sore throat, hoarse voice
The vocal cords are membranes at the entrance of the trachea that generate your voice. Inserting a tube into the trachea or the long-term tube placement may damage the vocal cords. This may cause a sore throat or hoarse voice when you wake up from anesthesia. Hoarseness can also be caused by arytenoid cartilage dislocation in your throat and should be diagnosed by a specialist.
It is less likely, but the damage by the tube can develop a vocal cord granuloma (swelling of the membrane) or paralyze the recurrent nerve that allows normal movement of the vocal cords. These conditions may cause difficulty speaking or coughing, which can take time to heal, and you may need to see a specialist for further treatment.
Pneumonia, aspiration pneumonia
If the contents of the stomach get into the trachea or lungs during or after anesthesia, severe pneumonia can develop. To prevent this lung complication, it is extremely important to refrain from eating and drinking before surgery.
Even with fasting, aspiration pneumonia related to anesthesia can occur in patients in certain conditions such as pregnancy, gastrointestinal obstructions, or abdominal tumors, or recent trauma.
Asthma attack or laryngeal spasms
Stimulation from inhalation anesthetics or tubes inserted into the throat as well as allergic reactions to drugs can cause bronchial spasms (asthma attack). This can happen to all people regardless of a history of asthma.
Laryngeal spasms can also occur, causing the vocal cords to close, obstructing breathing. An anesthesiologist will provides an immediate and appropriate treatment for these conditions.

This rare disease involves stiffening of the muscles and a high fever when exposed to certain anesthetics. The genes related to this disease are found in about 1 out of every 20,000 to 60,000 people. If any of your relatives have had abnormal reactions to anesthetics, please make sure to tell your doctor or anesthesiologist.
2. Complications that can occur during and/or after the anesthesia.
Pulmonary embolism
When a venous thrombus (blood clot) or an object blocks the blood vessels in the lungs, it can cause difficulty breathing, chest pain, and even cardiac arrest. This disease can be life-threatening. The main cause of pulmonary embolism is a thrombus formed from static blood in the lower limb veins, with or without hypercoagulability (the tendency of causing blood clots). This clot is called deep vein thrombosis, DVT. A higher risk of DVT is related to being bedridden for long periods, diseases that cause blood clots, obesity, pregnancy, the use of oral contraceptives, swollen legs, heart disease, malignant tumors, stroke, smoking, and other factors. Laparoscopic surgery, lower abdominal surgery, multiple fractures, and long surgeries are surgical factors associated with a higher risk of DVT. For prevention of DVT, wearing compression stockings, mechanical leg massagers (intermittent pneumatic compression devices), and other medical devices are recommended.
3. Complications of regional anesthesia
Headache
Puncture for spinal anesthesia can cause cerebrospinal fluid to leak from the needle hole in the dura mater, the membrane holding the cerebrospinal fluid. this leakage causes intracranial pressure to drop and can lead to severe headaches. This type of headache happens in about 0.5% of cases (one in every 170–200 people) and generally disappears in about a week without any treatment. To keep from getting a headache, rest as quietly as possible after returning to your room and do not make any sudden head movements. You may be told to drink plenty of water.
In some cases, the dura mater can be injured with epidural anesthesia procedure, and this injury causes similar headaches.
If your headache persists or worsens, please contact your medical team as soon as possible to rule out other causes and for further treatments.
Nerve injury, cauda equina syndrome or transient neurological signs
The spinal cord is a thick nerve cord continuing from the brain and ending at the level of the waist. The nerves inside the spinal column below this level is called the “cauda equina,” an area comprising many fine nerve threads. With spinal anesthesia, local anesthetics are injected into the area of cauda equina, and the needle does not normally damage the thick spinal cord trunk. Rarely, in roughly one in every 10,000 to 50,000 people, cauda equina syndrome occurs, which involves symptoms, such as sensory abnormalities in the lower half of the body, motor dysfunction, and dysfunction of the bladder and rectum. Leg pain and sensory abnormalities normally disappear within 24–72 hours (transient neurological signs); however, some symptoms may last longer in cauda equina syndrome.
Epidural hematoma, epidural abscess Subarachnoid hematoma, subarachnoid hematoma abscess
In patients with blood coagulation problems, inserting a needle or catheter into the spinal area or pulling out the catheter can cause a hematoma (blood collection) outside the dura mater, which can cause sensory or motor paralysis. Hematoma happens to about one in every 10,000 people. An epidural abscess occurs when bacteria enters and infect the epidural space Similar to a hematoma, an abscess puts pressure on nerves. Subarachnoid hematoma or abscess can also occur from spinal or epidural anesthesia.
Difficulty of urination
After epidural or spinal anesthesia wears off, you might feel the urge to urinate, be unable to do so. If this condition persists you may need temporary urinary catheter. Normally this resolves naturally, but if it persists, please seek medical attention.
Nausea, vomiting, itching, numbness of the legs by pain medications
Painkillers may cause nausea, vomiting, itching, and numbness of the legs. If this becomes unbearable, please notify your medical team.
Severing of a catheter
In rare cases, a catheter may break off with part of the catheter remaining in the body.
Please refer to your physician for further treatment.
Insufficient anesthesia
Regional anesthesia may not work well enough on the area intended. If surgery takes longer than expected, the effects of anesthesia may wear off prematurely. Your anesthesiologist may decide to switch to general anesthesia in these situations.
Local anesthetic toxicity
Local anesthetic toxicity can develop on the patient if the blood levels of the local anesthetics get too high. Local anesthetic toxicity can lead to arrhythmia (rapid or irregular heartbeats), coronary arterial spasms, unconsciousness, or even cardiac arrest, that need lifesaving treatment.
Difficulty of breathing caused by upper limb peripheral nerve block
Peripheral nerve block of the upper limbs may paralyze the diaphragm or cause pneumothorax (collapsed lung), making it difficult to breathe. Mechanical respiration might be necessary until the anesthetic effects on the diaphragm wears off, or a chest tube may need to be placed into the chest cavity for pneumothorax.
4. Perioperative complications
The risk of developing perioperative complications is higher in elderly patients and patients with underlying disease. In patient population with a history of underlying disease, i.e., heart disease (hypertension, arrhythmia, angina pectoris, myocardial infarction, etc.), lung disease (chronic obstructive lung disease, asthma, etc.), kidney disease or cerebrovascular disease (cerebral infarction or hemorrhage), these underlying diseases may worsen during the perioperative period. Two major perioperative complications are stroke and heart attack.
Intracranial hemorrhage, subarachnoid hemorrhage, cerebral infarction (Stroke)
Patients with a history of intracranial hemorrhage, subarachnoid hemorrhage, and hypertension have a higher risk of developing intracranial hemorrhage and/or subarachnoid hemorrhage following anesthesia. Patients with a history of arrhythmia and cerebral infarction have a higher risk of developing cerebral infarction following anesthesia.
Acute coronary syndrome (Heart attack)
Patients with a history of heart failure, angina pectoris, hypertension, diabetes, cerebral infarction, and/or kidney disease, have a higher risk of acute coronary syndrome following anesthesia. Patients with a history of myocardial infarction have an even higher risk.
5. Preventing complications
Most of the complications of anesthesia are preventable through careful management based on appropriate preoperative assessment and planning by your anesthesiologist.
However, it should be noted that, like any other medical practice, anesthesia itself cannot be 100%-safe even if all the appropriate steps are taken. Your anesthesiologist is responsible for your anesthesia and does everything possible to provide you with anesthetic care at the highest levels of safety throughout the perioperative period.
6. Emergency anesthetic procedures
All of these emergency procedures are aimed at saving the patient's life.
Treatments that may be performed during an emergency without prior explanation include the following.
- Tracheotomy or preparations for this procedure
- Open or closed cardiac massage or chest compression
- Use of a defibrillator (shock)
- Blood transfusion without a cross-matching test
- Other necessary life-saving procedures
Afterword
We hope this Patient's Guide to Anesthesia will help you and your family gain a better understanding of anesthesia, and also hope that this Guide will relieve concerns and worries about anesthesia of you and your family.
Anesthetic care should be provided with the best available safety. Based on this belief , the JSA continuously aims to help all medical providers prevent unforeseen complications related to anesthesia and surgical/medical procedures. Your anesthesiologist works closely with your surgeons, , other doctors, nurses, pharmacists, and other medical personnel, in order to give you the best possible anesthetic care to promote the fastest recovery. Please feel free to ask your anesthesiologist any question about anesthesia.
Published October 2006
Revised June 2012
Revised August 2013
Revised September 2015
Revised March 2017
Revised June 2018
Revised October 2020
Publisher: Japanese Society of Anesthesiologists
Editor: Japanese Society of Anesthesiologists, Public Relations Committee
English version: October 2020
Editors for English Version: Japanese Society of Anesthesiologists, Committee on International Affairs
For inquiries, please contact us through our website.
URL: http://www.anesth.or.jp/
©2019 Japanese Society of Anesthesiologists